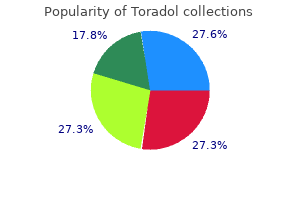
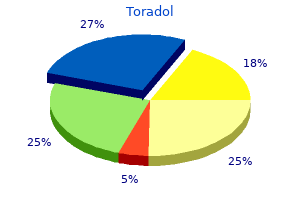
Toradol dosages: 10 mg
Toradol packs: 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills

Generic 10mg toradol visa
The assessment of glomerular filtration is fundamental to the diagnosis of renal glomerular pathology and the administration of drug remedy pain treatment center memphis toradol 10mg visa, where clearance is determined by the glomerular filtration joint and pain treatment center lompoc ca buy toradol 10mg lowest price, and in chronic kidney illness to facilitate timely management selections backbone pain treatment yoga order toradol 10 mg amex. The ideal marker is endogenous pain medication for glaucoma in dogs cheap toradol 10mg without prescription, freely filtered by the glomerulus, neither reabsorbed nor secreted by the renal tubule, and eradicated only by the kidney. Rapid removal of ions from the renal medulla by the circulation of blood is minimized by one other looped countercurrent system. This is the countercurrent exchange mechanism, in which arterioles getting into the medulla pass for long distances parallel to the venules leaving it, earlier than ending in capillary beds around tubules. Concentration of urine Because sodium and chloride ions are selectively resorbed by the cells of the ascending limbs and distal tubules beneath aldosterone management, the filtrate at the distal end of the convoluted tubules is hypotonic. As it reaches the amassing ducts, fluid descends once more by way of the medulla and, thus, re-enters a region of excessive osmotic strain. This complicated system is very flexible and the steadiness between the rate of filtration and absorption can be various to meet present physiological demands. Control of hydrogen and ammonium ion concentrations is essential to the regulation of acids and bases in the blood. Over 91% of ingested potassium is excreted in urine, largely through secretion by cells of the distal tubule and accumulating duct. The components of a juxtaglomerular apparatus are juxtaglomerular and lacis cells, and the macula densa. The cells of the tunica media of afferent and, to a lesser extent, efferent, arterioles differ from typical easy muscle cells. These juxtaglomerular cells are large, rounded, myoepithelioid cells and their cytoplasm contains many mitochondria and dense, renin-containing vesicles, 10�40 nm in diameter. Each macula densa of the distal tubule is a cluster of up to 40 tightly packed cells in the tubule wall; the cells have Selective resorption Selective resorption from the filtrate is an active process and occurs primarily in the proximal convoluted tubules, which resorb glucose, amino acids, phosphate, chloride, sodium, calcium and bicarbonate, and take up small proteins. Cells of the proximal tubules are permeable to water, which passes out of the tubules passively, in order that the filtrate stays locally isotonic with blood. They are osmoreceptors, sensing the NaCl content of the filtrate after its passage through the loop of Henle. When NaCl concentrations in the filtrate change, tubuloglomerular suggestions mechanisms function to maintain the inverse relationship between salt focus and glomerular filtration price. Macula densa cells are thought to respond to excessive salt concentration in the distal tubule by releasing nitric oxide, which inhibits the tubuloglomerular feedback response and reduces filtration fee. The position of macula densa cells in the stimulation of renin release to increase filtration fee is much less nicely understood. The third factor of the juxtaglomerular apparatus is a inhabitants of extraglomerular mesangial cells that kind a network (or lace; hence, their alternative name of lacis cells) of stellate cells connecting the macula densa sensory cells with the juxtaglomerular effector cells. It is likely that extraglomerular mesangial cells transmit the sensory sign, possibly via hole junctions. They can also signal to contractile glomerular mesangial cells and impact vasoconstriction directly throughout the glomerulus. Each measures 25�30 cm in length, is thick-walled and slender, and is continuous superiorly with the funnel-shaped renal pelvis. Each descends barely medially, anterior to psoas major, and enters the pelvic cavity, where it curves initially laterally, then medially, to open into the base of the urinary bladder. The diameter of the ureter is generally three mm, however is barely less at its junction with the renal pelvis, at the brim of the lesser pelvis near the medial border of psoas main, and where it runs inside the wall of the urinary bladder, which is its narrowest half. During surgical procedure on intraperitoneal constructions, the ureter could be tented up because the peritoneum is drawn anteriorly, resulting in inadvertent ureteric damage. Anterior to psoas major, it crosses anterior to the genitofemoral nerve and is obliquely crossed by the gonadal vessels. The inferior vena cava is medial to the best ureter, whereas the left ureter is lateral to the aorta. The inferior mesenteric vein has an extended retroperitoneal course lying near the medial facet of the left ureter. At its origin, the best ureter is often overlapped by the descending part of the duodenum. It descends lateral to the inferior vena cava, and is crossed anteriorly by the right colic and ileocolic vessels.

Buy toradol 10mg
The two heavy chains wrap spirally round each other to kind a double helix groin pain treatment exercises 10mg toradol sale, which known as the tail of the myosin molecule pain medication for shingles nerves cheap toradol 10mg on-line. One end of every of these chains is folded bilaterally into a globular polypeptide construction referred to as a myosin head pain treatment center bethesda md 10mg toradol with mastercard. Relaxed and contracted states of a myofibril displaying (top)slidingoftheactinfilaments(pink)intothespacesbetweenthe myosin filaments (red) and (bottom) pulling of the Z membranes towardeachother joint pain treatment in ayurveda purchase toradol 10mg with amex. Also, a part of the physique of every myosin molecule hangs to the aspect along with the top, thus providing an arm that extends the pinnacle outward from the physique, as shown within the determine. Each cross-bridge is flexible at two factors referred to as hinges-one where the arm leaves the physique of the myosin filament, and the other the place the top attaches to the arm. The hinged arms enable the heads to be both extended far outward from the body of the myosin filament or brought near the body. The hinged heads in flip participate within the actual contraction course of, as mentioned within the following sections. Now, to full the picture, the myosin filament is twisted so that each successive pair of cross-bridges is axially displaced from the earlier pair by 120 levels. This twisting ensures that the cross-bridges lengthen in all directions around the filament. The lively sites on the two F-actin strands of the double helix are staggered, giving one active website on the overall actin filament about every 2. Each molecule of tropomyosin has a molecular weight of 70,000 and a size of 40 nanometers. The backbone of the actin filament is a intermittently along the edges of the tropomyosin molecules are additional protein molecules called troponin. These protein molecules are literally complexes of three loosely certain protein subunits, each of which plays a particular position in controlling muscle contraction. One of the subunits (troponin I) has a robust affinity for actin, one other (troponin T) for tropomyosin, and a 3rd (troponin C) for calcium ions. The sturdy affinity of the troponin for calcium ions is believed to provoke the contraction process, as defined in the subsequent part. Active websites Troponin advanced Interaction of One Myosin Filament, Two Actin Filaments, and Calcium Ions to Cause Contraction Inhibition of the Actin Filament by the TroponinTropomyosin Complex. Actin filament, composed of two helical strands of F-actin molecules and two strands of tropomyosin molecules that match within the grooves between the actin strands. Attached to one end of each tropomyosin molecule is a troponin complicated that initiates contraction. Before contraction can happen, the inhibitory impact of the troponin-tropomyosin complex must itself be inhibited. In the presence of huge amounts of calcium ions, the inhibitory impact of the troponin-tropomyosin on the actin filaments is itself inhibited. This motion "uncovers" the lively sites of the actin, thus permitting these energetic websites to attract the myosin cross-bridge heads and cause contraction to proceed. Although this mechanism is hypothetical, it does emphasize that the conventional relation between the troponin-tropomyosin advanced and actin is altered by calcium ions, producing a brand new condition that leads to contraction. Interaction of the "Activated" Actin Filament and the Myosin Cross-Bridges-The "Walk-Along" Theory of Contraction. As soon as the actin filament is activated a new energy stroke, and the actin filament strikes one other step. Thus, the heads of the cross-bridges bend backwards and forwards and step-by-step stroll alongside the actin filament, pulling the ends of two successive actin filaments towards the center of the myosin filament. Each one of the cross-bridges is believed to operate independently of all others, every attaching and pulling in a steady repeated cycle. Therefore, the higher the number of cross-bridges in touch with the actin filament at any given time, the greater the force of contraction. When a by the calcium ions, the heads of the cross-bridges from the myosin filaments become attracted to the lively sites of the actin filament, and this, ultimately, causes contraction to happen. Although the precise manner by which this interplay between the cross-bridges and the actin causes contraction is still partly theoretical, one hypothesis for which considerable proof exists is the "walkalong" (or "ratchet") principle of contraction. The figure exhibits the heads of two cross-bridges attaching to and disengaging from energetic websites of an actin filament. When a head attaches to an lively site, this attachment concurrently causes profound changes in the intramolecular forces between the head and arm of its cross-bridge.
Buy discount toradol 10mg online
The deliberate division of the perineal physique to facilitate delivery (episiotomy) is usually angled laterally to keep away from such sphincteric injuries pain treatment after knee replacement discount toradol 10mg without prescription. The perineal physique is commonly used to position radiological markers within the evaluation of pelvic ground dysfunction pain medication for dogs surgery buy toradol 10mg cheap. A few fibres may cross into the ipsilateral bulbospongiosus or exterior anal sphincter allied pain treatment center investigation purchase toradol 10 mg overnight delivery. The tissue commonly referred to because the deep perineal fascia is a layer of fascia that overlies the superficial muscle tissue of the perineum (bulbospongiosus midsouth pain treatment center reviews purchase 10 mg toradol overnight delivery, ischiocavernosus, superficial transverse perineal muscles). It is, in impact, the investing fascia of the superficial perineal muscular tissues and, as such, is firmly attached to the borders of the muscular tissues at attachments to the ischiopubic rami, posterior margin of the perineal membrane and perineal body. Anteriorly, it fuses with the suspensory Bulbospongiosus Bulbospongiosus differs between the sexes. The fibres attach to the perineal body, by which they decussate, and to the transverse superficial perinei and the external anal sphincter; they diverge like the edges of a feather from the median raphe. A thin layer of posterior fibres joins the posterior portion of the perineal membrane. The anterior fibres spread out over the edges of the corpora cavernosa, ending partly in them, anterior to ischiocavernosus, and partly in a tendinous enlargement that covers the dorsal vessels of the penis. Fibres run anteriorly on either side of the vagina to connect to the corpora cavernosa clitoridis, and a few fibres cross over the dorsum of the body of the clitoris. The canal lies about four cm above the lower limit of the ischial tuberosity and is fashioned by connective tissue binding the vessels and nerve to the medial floor of the fascia covering obturator internus. As the artery approaches the margin of the ischial ramus, it proceeds above or below the perineal membrane, alongside the medial margin of the inferior pubic ramus, en path to its target buildings. Given its distribution, the inner pudendal artery distal to its perineal department has been named the artery of the penis. The artery to the bulb provides the corpus spongiosum, and the cavernous artery of the penis supplies the corpus cavernosum on all sides. The dorsal artery runs on the dorsal aspect of the penis and supplies circumflex branches to the corpora cavernosa and corpus spongiosum that end by anastomosing in the coronal sulcus and supplying the glans penis and its overlying pores and skin. In the female, a similar branch of the pudendal artery is distributed to the erectile tissue of the corpus spongiosum and vagina. The cavernous artery supplies the corpora cavernosa of the clitoris; the dorsal artery supplies the glans and prepuce of the clitoris. Branches of the inner pudendal artery are typically derived from an adjunct pudendal artery, which is normally a branch of the pudendal artery before its exit from the pelvis; effectively, the artery is double earlier than it leaves the pelvis. It might help in the last stage of erection as the middle fibres compress the erectile tissue of the bulb and the anterior fibres contribute by compressing the deep dorsal vein of the penis. It contracts six or seven instances during ejaculation, helping within the expulsion of semen. In the feminine, bulbospongiosus acts to constrict the vaginal orifice and express the secretions of the larger vestibular glands. Anterior fibres contribute to erection of the clitoris by compressing its deep dorsal vein. The muscle tissue form a triangle on each side of the midline with bulbospongiosus medially and the superficial transverse perineal muscle tissue posteriorly, hooked up to the perineal membrane; when contracted, the two ischiocavernosi act collectively to stabilize the erect penis. In the feminine, ischiocavernosus might assist to promote increased strain in the clitoris. Inferior rectal artery the inferior rectal artery arises just after the interior pudendal artery enters the pudendal canal on the lateral wall of the ischio-anal fossa. Perineal artery the perineal artery is a department of the interior pudendal artery that arises close to the anterior end of the pudendal canal and runs via the perineal membrane. A small transverse department passes medially, inferior to the superficial transverse perineal muscle, to anastomose with the contralateral artery and with the posterior scrotal and inferior rectal arteries. It supplies the transverse perinei, the perineal physique and the posterior attachment of the bulb of the penis. The posterior scrotal arteries are often terminal branches of the perineal artery however can also come up from its transverse branch. They are distributed to the scrotal pores and skin and dartos muscle within the male and provide the perineal muscular tissues. Veins of the perineum: internal pudendal veins the inner pudendal veins are venae comitantes of the inner pudendal artery and unite as a single vessel ending within the internal iliac vein.

Buy toradol 10mg without a prescription
This motion is brought on by forces generated by interaction of the cross-bridges from the myosin filaments with the actin filaments joint and pain treatment center fresno ca toradol 10mg without prescription. The new alignment of forces causes the pinnacle to tilt toward the arm and to drag the actin filament along with it xiphoid pain treatment purchase 10 mg toradol otc. Immediately after tilting pain treatment for uti quality toradol 10mg, the top then mechanically breaks away from the lively web site chest pain treatment protocol cheap 10 mg toradol. The following sequence of events is believed to be the means by which this effect occurs: 1. The bond between the top of the cross-bridge and the active site of the actin filament causes a conformational change within the head, prompting the head to tilt toward the arm of the cross-bridge and offering the facility stroke for pulling the actin filament. That is, the power again "cocks" the head back to its perpendicular situation, ready to start the new power stroke cycle. Thus, the process proceeds many times until the actin filaments pull the Z membrane up in opposition to the ends of the myosin filaments or till the load on the muscle turns into too great for further pulling to happen. To the best are totally different degrees of overlap of the myosin and actin filaments at different sarcomere lengths. At point D on the diagram, the actin filament has pulled all the way out to the top of the myosin filament, with no actinmyosin overlap. Then, as the sarcomere shortens and the actin filament begins to overlap the myosin filament, the strain increases progressively until the sarcomere size decreases to about 2. At this point, the actin filament has already overlapped all the cross-bridges of the myosin filament however has not but reached the middle of the myosin filament. With further shortening, the sarcomere maintains full rigidity till point B is reached, at a sarcomere size of about 2 micrometers. At this point, the ends of the two actin filaments begin to overlap one another along with overlapping the myosin filaments. At this point, the 2 Z disks of the sarcomere abut the ends of the myosin filaments. However, the increase in rigidity that happens during contraction, called active pressure, decreases because the muscle is stretched past its regular length-that is, to a sarcomere size higher than about 2. This phenomenon is demonstrated by the decreased size of the arrow within the determine at larger than normal muscle size. Relation of Velocity of Contraction to Load A skeletal muscle contracts quickly when it contracts towards no load-to a state of full contraction in about zero. This lowering velocity of contraction with load is caused by the fact that a load on a contracting muscle is a reverse drive that opposes the contractile force caused by muscle contraction. To perform work signifies that power is transferred from the muscle to the external load to lift an object to a higher height or to overcome resistance to movement. In mathematical phrases, work is outlined by the following equation: W = L �D by which W is the work output, L is the load, and D is the gap of movement in opposition to the load. The power required to carry out the work is derived from the chemical reactions within the muscle cells during contraction, as described within the following sections. However, so many finish merchandise of glycolysis accumulate in the muscle cells that glycolysis additionally loses its functionality to sustain most muscle contraction after about 1 minute. More than ninety five percent of all energy used by the muscular tissues for sustained, long-term contraction is derived from oxidative metabolism. For extremely long-term maximal muscle activity-over a period of many hours-by far the greatest proportion of energy comes from fats, but for durations of 2 to 4 hours, as a lot as one half of the vitality can come from saved carbohydrates. Velocity of contraction (cm/sec) Chapter 6 ContractionofSkeletalMuscle the detailed mechanisms of those energetic processes are discussed in Chapters 67 via 72. In addition, the importance of the completely different mechanisms of vitality release during performance of various sports is mentioned in Chapter eighty four. The proportion of the input power to muscle (the chemical energy in nutrients) that can be converted into work, even under one of the best circumstances, is less than 25 p.c, with the rest changing into heat. Maximum effectivity can be realized solely when the muscle contracts at a reasonable velocity. If the muscle contracts slowly or with none motion, small amounts of upkeep heat are released during contraction, despite the very fact that little or no work is performed, thereby reducing the conversion efficiency to as little as zero.
Buy cheap toradol 10mg line
The iliofemoral ligament is the strongest pain treatment pancreatitis buy toradol 10mg with visa, and is progressively tightened when the femur extends to the road of the trunk pain medication for dogs surgery generic 10mg toradol with mastercard. The pubofemoral and ischiofemoral ligaments also tighten when this occurs and chronic pelvic pain treatment guidelines discount toradol 10 mg amex, because the joint approaches the close-packed position stomach pain treatment home toradol 10 mg without prescription, resistance to an extending torque will increase rapidly. The transverse acetabular ligament and ligament of the head of the femur also contribute to stability. Only slight separation of the articular surfaces may be achieved by sturdy traction on the joint. To assist insertion of an arthroscope, a needle is first inserted into the joint to remove the suction effect; the joint will subsequently open sufficiently with traction. Traumatic dislocation usually occurs solely when the joint is subjected to extreme drive. Synovial membrane Starting from the femoral articular margin, the synovial membrane covers the intracapsular a half of the femoral neck, after which passes to the interior floor of the capsule to cover the acetabular labrum, the ligament of the pinnacle of femur and fats within the acetabular fossa. The biomechanical options of the human decrease limb, whose function is primarily to enable stance and bipedal propulsion, are very completely different from those of the quadruped decrease limb, and these variations are reflected in the anatomy and biomechanics of the human hip, knee, ankle and foot joints. This articulation is innately limited in its capability for translational movement in anteroposterior, transverse and vertical instructions. Bursae the hip joint could communicate with the subtendinous iliopectineal bursa by way of a circular aperture between the pubofemoral ligament and the descending a part of the iliofemoral ligament. More distant bursae are related to the tendons of distal attachment of glutei medius and minimus at the larger trochanter, and between gluteus maximus and vastus lateralis. Femur the femur is actually a tubular construction with distortions that consist of bows and twists. The most notable is the anterior bow in its mid portion, the place the radius of curvature is relatively constant alongside the length of the femoral shaft. Although the neck�shaft angle (collo�diaphyseal angle; Mikulicz angle) and neck length are variable, the centre of the neck within the coronal plane is at the degree of the apex of the larger trochanter. As the kid develops, forces from muscular tissues and gravity cause the angle of anteversion to lower gradually, approaching 15� by young adulthood. Lymphatics from the anterior facet of the hip joint drain to the deep inguinal nodes, while these from the medial and posterior features of the joint journey with the obturator and gluteal arteries, respectively, to reach the interior iliac nodes. The posterior capsule is innervated by the sciatic and superior gluteal nerves, and by the nerve to quadratus femoris (Birnbaum et al 1997, Gardner 1948). Head N Neck B Greater trochanter Hip and groin pain Pain emanating from the hip and groin has many potential causes. Pain over the lateral facet of the hip usually suggests a neighborhood drawback such as trochanteric bursitis. Attritional persistent overload of the anterior stomach wall at its attachments to the pubis and inguinal ligament, or of exterior indirect at the superficial inguinal ring, is a typical occurrence. In addition, in most hips, a line nearly perpendicular to S from the tip of the higher trochanter (B) passes by way of the centre of the femoral head. This approximation can be utilized in judging the position of the femoral osteotomy in hip arthroplasty. Since the growth plate is avascular, the one blood provide to the femoral head is conveyed via the retinacular vessels, which are mainly tributaries of the medial circumflex femoral artery. These retinacular arteries enter the joint capsule in the trochanteric fossa and ascend the femoral neck on its outer side superiorly and posteriorly. A minor contribution to the vascular provide comes from the ligament of the head of the femur. The yellow arrow reveals posterior displacement of the femoral head in the slipped capital femoral epiphysis. The purple arrow indicates the course of the retinacular vessels along the posterior aspect of the femoral neck. The body subsequently tends to incline posteriorly but that is counterbalanced by ligamentous pressure and congruence and compression of the articular surfaces within the hip joints in the close-packed position. Under increased loading of the trunk or leaning posteriorly, these resistive however passive factors are assisted by energetic force produced by the hip joint flexors. In swaying anteriorly on the ankles, or when the arms are stretched forwards, and in addition in forward-bending at the hip, the line of physique weight moves anterior to the medial�lateral axis of rotation by way of the hip joints. The posture adopted, or the speed of change of posture, is largely controlled by the hamstrings, which, apart from being highly effective flexors of the knee, are strong extensors of the hip.
Purchase toradol 10 mg free shipping
A more distal nerve entrapment syndrome causing chronic medial thigh ache has been described in athletes with giant adductor muscle tissue pain treatment for labor buy toradol 10 mg. Vascular branches of the femoral nerve supply the femoral artery and its branches joint and pain treatment center thousand oaks purchase 10 mg toradol with amex. Sometimes the accent obturator nerve could be very small and only supplies pectineus advanced diagnostic pain treatment center new haven generic 10 mg toradol fast delivery. Any department may be absent and others might happen; a further branch generally supplies adductor longus pain treatment medication toradol 10mg on-line. Sciatic nerve the sciatic nerve is 2 cm extensive at its origin and is the thickest nerve within the body. Superiorly, it lies deep to gluteus maximus, resting first on the posterior ischial floor with the nerve to quadratus femoris between them. It then crosses posterior to obturator internus, the gemelli and quadratus femoris, separated by the latter from obturator externus and the hip joint. It is accompanied medially by the posterior femoral cutaneous nerve and the inferior gluteal artery. More distally, it lies behind adductor magnus and is crossed posteriorly by the long head of biceps femoris. Its course corresponds to a line drawn from simply medial to the midpoint between the ischial tuberosity and higher trochanter to the apex of the popliteal fossa. Articular branches come up proximally to provide the hip joint by way of its posterior capsule; these are generally derived immediately from the sacral plexus. Muscular branches are distributed to biceps femoris, semitendinosus, semimembranosus and the ischial a half of adductor magnus. The point of division of the sciatic nerve into its tibial and customary fibular elements may be very variable. The widespread site is on the junction of the center and decrease thirds of the thigh, close to the apex of the popliteal fossa, but the division could occur at any stage above this point and, rarely, may happen under it. Lower in the thigh, arterial branches derived from the perforating branches of the profunda femoris artery or the anastomotic chain between them or, often, from the popliteal artery, enter the nerve on its lateral or anterolateral aspect (Sunderland 1945). The numerous arterial branches to the sciatic nerve anastomose with one another to form extraneural and intraneural arterial chains (Sunderland 1945, Ugrenovic et al 2013). Lateral dorsal cutaneous nerve Medial and lateral plantar nerves 80 Pelvic girdle, gluteal region and thigh sciatic nerve palsy could be very rare. As it leaves the pelvis, it passes either behind piriformis or typically by way of the muscle, and at that point it may very rarely turn out to be entrapped or tethered; the piriformis syndrome is a controversial condition in which an anomalous relationship between piriformis and the sciatic nerve is thought to cause ache in the buttocks and alongside the course of the sciatic nerve. However, the most common trigger of serious sciatic nerve damage (and of the resulting major medicolegal claims) is iatrogenic (Dillow et al 2013). The nerve may be broken in misplaced therapeutic injections into gluteus maximus. Sciatic nerve palsy happens after whole hip substitute or similar surgery in 1% of instances, and may be caused by sharp harm, burning from bone cement, traction from devices, manipulation of the hip, inadvertent lengthening of the femur, or haematoma surrounding the nerve. For some cause, presumably anatomical, the widespread fibular component of the sciatic nerve is extra normally affected; the affected person has a foot drop and a high-stepping gait. Nerve to obturator internus the nerve to obturator internus arises from the ventral branches of the fifth lumbar and first and second sacral ventral rami. It leaves the pelvis by way of the larger sciatic foramen under piriformis, supplies a branch to the upper posterior surface of gemellus superior, crosses the ischial spine lateral to the internal pudendal vessels, re-enters the pelvis via the lesser sciatic foramen, and enters the pelvic surface of obturator internus. Posterior femoral cutaneous nerve (posterior cutaneous nerve of the thigh) the posterior femoral cutaneous nerve (posterior cutaneous nerve of the thigh) arises from the dorsal branches of the primary and second, and the ventral branches of the second and third sacral rami. It descends at the back of the thigh superficial to the long head of biceps femoris, deep to the fascia lata. It pierces the deep fascia behind the knee and accompanies the short saphenous vein to mid-calf, its terminal twigs connecting with the sural nerve. Its branches are cutaneous and are distributed to the gluteal region, perineum, posterior thigh and proximal posterior leg.
Cheap toradol 10 mg with amex
The phrenicocolic ligament connects the splenic flexure of the colon to the diaphragm and runs inferior and lateral to the decrease pole of the spleen treatment for uti back pain purchase toradol 10mg. It is continuous with the peritoneum of the lateral finish of the transverse mesocolon on the end of the pancreatic tail midwest pain treatment center wausau wi generic toradol 10mg with visa, and the splenorenal ligament at the hilum of the spleen (Merchea et al 2012 pain treatment center northside hospital discount toradol 10mg with mastercard, Skandalakis et al 1993) pain treatment back generic toradol 10mg free shipping. When the phrenicocolic ligament is being divided, particularly when electrocautery is used, the colon is susceptible to injury. Mobile spleen the length of the peritoneal ligaments associated with the spleen differ; longer ligaments afford the spleen larger mobility, which may stretch its vascular pedicle. This facilitates surgical mobilization but could render the spleen more vulnerable to injury from shear forces during trauma. A floating or wandering spleen is characterized by extreme mobility and migration of the organ outdoors the left hypochondrium. Mobilization of the spleen requires division of the phrenicocolic, gastrosplenic and phrenicosplenic ligaments. Undue traction on the phrenicocolic ligament throughout mobilization of the splenic flexure might tear the splenic capsule, causing bleeding (Merchea et al 2012). This is less likely if the phrenicocolic ligament is retracted laterally somewhat than inferiorly and medially (Merchea et al 2012). The anterosuperior border and anterior diaphragmatic surface of the spleen are sometimes adherent to the higher omentum and care must be taken when retracting the latter. The diaphragmatic floor of the spleen is occasionally adherent to the peritoneum on the undersurface of the diaphragm; these adhesions may comply with inflammation of the spleen or be congenital in origin (Petroianu 2011, Skandalakis et al 1993). Almost always, the splenic artery arises from the coeliac trunk, in common with the left gastric and common hepatic arteries. However, it might originate from the common hepatic artery or the left gastric artery, or not often instantly from the aorta either in isolation or as a splenomesenteric trunk (Cort�s and Pellico 1988, Garc�a-Porrero and Lemes 1988, Liu et al 1996, Pandey et al 2004, Torres 1998, Trubel 1985). From its origin, the artery runs a little means inferiorly earlier than turning to the left behind the abdomen to run horizontally posterior to the higher border of the body and tail of the pancreas. Multiple loops and even coils of the artery appear above the superior border of the pancreas (McFee et al 1995, Pandey et al 2004). The splenic artery courses anterior to the left kidney and left suprarenal gland, and runs within the splenorenal ligament behind or above the tail of the pancreas. In its course, it gives off quite a few branches to the pancreas (dorsal pancreatic, greater pancreatic artery, and arteries to the tail) and, close to its termination, it gives off the short gastric arteries and the left gastroepiploic artery (G�rleyik et al 2000, Liu et al 1996, Mikhail et al 1979, Pandey et al 2004, Skandalakis et al 1993, Trubel et al 1985, Trubel et al 1988). Additional branches embody a posterior gastric artery in 40% of people and small retroperitoneal branches. The splenic artery varies between eight and 32 cm in length and its calibre usually exceeds that of the widespread hepatic and left gastric arteries, starting from 3 to 12 mm. Splenic artery blood move is approximately three ml/sec/100 g, corresponding to approximately 7% of cardiac output (Cort�s and Pellico 1988, Garc�a-Porrero and Lemes 1988, Nakamura et al 1989, Pandey et al 2004, Petroianu 2011, Skandalakis et al 1993, Torres 1998, Trubel et al 1985). The splenic artery normally divides into two, or sometimes three, branches before getting into the hilum of the spleen. The superior and inferior branches are generally often known as superior and inferior polar arteries; as they enter the hilum they divide into four or five segmental arteries that every provide a segment of splenic tissue. There is comparatively little arterial collateral circulation between segments, which implies that occlusion of a segmental vessel often results in infarction of a half of the spleen (Cort�s and Pellico 1988, Garc�a-Porrero and Lemes 1988, Gupta et al 1976, Liu et al 1996, Mikhail et al 1979, Pandey et al 2004, Torres 1998, Trubel al 1985, Trubel et al 1988). Segmental arteries divide throughout the splenic trabeculae and provides rise to follicular arterioles, that are surrounded by a thick lymphoid sheath of white pulp. There is considerable communication between arterioles (Garc�a-Porrero and Lemes 1988, Liu et al 1996, Mikhail et al 1979, Skandalakis et al 1993, Sow et al 1991, Trubel et al 1988). The superior pole of the spleen gains an extra arterial provide, distinct from the splenic hilar vessels, from the short gastric arteries in the gastrosplenic ligament. These vessels connect the superior pole of the spleen to the gastric fundus and preserve viability of this area of the spleen after ligation of the splenic pedicle (Garc�a-Porrero and Lemes 1988, G�rleyik et al 2000, Liu et al 1996, Petroianu 2011, Petroianu and Petroianu 1994, Petroianu et al 1989, Skandalakis et al 1993, Torres 1998, Trubel et al 1988). Communicating veins may interconnect lobar veins (DeLand 1970, Gupta et al 1980, Liu et al 1996, Par et al 1965, Sow et al 1991).
Discount toradol 10 mg line
The meniscofemoral ligaments are believed to act as secondary restraints midsouth pain treatment center cordova tn order 10 mg toradol fast delivery, supporting the posterior cruciate ligament in minimizing displacement brought on by posteriorly directed forces on the tibia pain treatment for pleurisy buy generic toradol 10mg on-line. These ligaments are additionally involved in controlling the motion of the lateral meniscus in conjunction with the tendon of popliteus throughout knee flexion allied pain treatment center youngstown oh order toradol 10mg with amex. Layer 1 Layer 1 is probably the most superficial and is the deep fascia that invests sartorius home treatment for shingles pain cheap 10mg toradol with visa. The saphenous nerve and its infrapatellar department are superficial to the deep fascia of the leg. Sartorius inserts into the fascia as an expansion quite than as a definite tendon. The fascia spreads inferiorly and anteriorly to lie superficial to the distinct and readily identifiable tendons of gracilis and semitendinosus and their insertions. The latter two tendons are generally harvested for surgical reconstruction of damaged cruciate ligaments. Deep to the tendons is the anserine bursa, which overlies the superficial part of the tibial collateral ligament; this bursa typically becomes inflamed, particularly in observe and area athletes. Posteriorly, layer 1 overlies the tendons of gastrocnemius and the structures of the popliteal fossa. Anteriorly, layer 1 blends with the anterior limit of layer 2 and the medial patellar retinaculum. A condensation of tissue passes from the medial border of the patella to the medial epicondyle of the femur (the medial patellofemoral ligament), the anterior horn of the medial meniscus (the meniscopatellar ligament), and the medial tibial condyle (the patellotibial ligament). Capsule and retinacula the joint capsule is a fibrous membrane of variable thickness. Elsewhere, it lies deep to expansions from vasti medialis and lateralis, separated from them by a airplane of vascularized unfastened connective tissue. The expansions are hooked up to the patellar margins and patellar ligament, extending back to the corresponding collateral (tibial and fibular) ligaments and distally to the tibial condyles. They kind medial and lateral patellar retinacula, the lateral being bolstered by the iliotibial tract. Posteriorly, the capsule accommodates vertical fibres that come up from the articular margins of the femoral condyles and intercondylar fossa, and from the proximal tibia. The oblique popliteal ligament is a well-defined thickening across the posteromedial side of the capsule, and is among the main extensions from the tendon of semimembranosus. The superficial part of the tibial collateral ligament has vertical and oblique portions. The former incorporates vertically oriented fibres that pass from the medial epicondyle of the femur to a big insertion on the medial surface of the proximal finish of the tibial shaft. Its anterior edge is rolled and easily seen simply posterior to the insertions of gracilis and semitendinosus once layer 1 has been opened. The posteriorly placed oblique fibres run posteroinferiorly from the medial epicondyle of the femur to mix with the underlying layer three (capsule), effectively to insert on the posteromedial tibial articular margin and posterior horn of the medial meniscus. There is a vertical break up in layer 2 anterior to the superficial a part of the tibial collateral ligament. The fibres anterior to the break up cross superiorly to mix with vastus medialis fascia and layer 1 within the medial patellar retinaculum. The fibres posterior to the cut up pass superiorly to the medial epicondyle and thence anteriorly because the medial patellofemoral ligament. Layer three Layer 3 is the capsule of the knee joint and may be separated from layer 2 in all places except anteriorly near the patella, where it blends with the extra superficial layers. Anteriorly, the separation of the superficial and deep parts of the tibial collateral ligament is distinct. The latter is thicker and subdivided into three components: the lateral patellofemoral ligament, operating from the lateral patellar border to the lateral epicondyle of the femur; the transverse retinaculum, operating from the iliotibial tract to the mid-patella; and the patellotibial band, operating from the patella to the lateral tibial condyle. The fascia lata and the iliotibial tract lie posterior to the lateral retinaculum. Here, because it emerges from behind the biceps femoris tendon, the frequent fibular nerve lies in a thin layer of fats sure by the fascia.
References
- Malone DL, Hess JR, Fingerhut A. MT practices around the globe and a suggestion for a common MT protocol. J Trauma. 2006;60:S91-S96.
- Werman HA, Falcone RE: Glottic positioning of the endotracheal tube tip: a diagnostic dilemma. Ann Emerg Med 31:643, 1998.
- Patel CR, Lane JR, Muise KL: In utero diagnosis of obstructed supracardiac total anomalous pulmonary venous connection in a patient with right atrial isomerism and asplenia. Ultrasound Obstet Gynecol 2001; 17:268-271.
- Henderson JF, Kelley WN, Rosenbloom FM, Seegmiller JE. Inheritance of purine phosphoribosyltransferase in man. Am J Hum Genet 1969;21:61.
- Repici A, Conio M, Angelis C, et al: Temporary placement of an expandable polyester silicone-covered stent for treatment of refractory benign esophageal strictures. Gastrointest Endosc 60:513, 2004.
- Lara-Hernandez R, Lozano-Vilardell P, Blanes P, et al: Safety and efficacy of therapeutic angiogenesis as a novel treatment in patients with critical limb ischemia, Ann Vasc Surg 24:287-294, 2010.

